The Situation
The Dayton Board of Education, with an average of 3,438 monthly members, had an annual pharmacy plan spend of $5.8 million. Unfortunately, the board’s overall pharmacy spending trend had increased steadily from $95.84 per member per month (PMPM) in the first quarter to $164.44 PMPM in the fourth quarter – averaging $141.14 PMPM for the year. Facing these increased costs, the board needed a strategic pharmacy benefits partner who could implement targeted, clinically based pharmacy savings programs and provide ongoing guidance to help lower their annual pharmacy spend in a sustainable way.

The Solution
The Dayton school board worked with RxBenefits’ expert clinical team to apply the following Protect components to address the plan’s top risk areas and decrease pharmacy benefits costs:
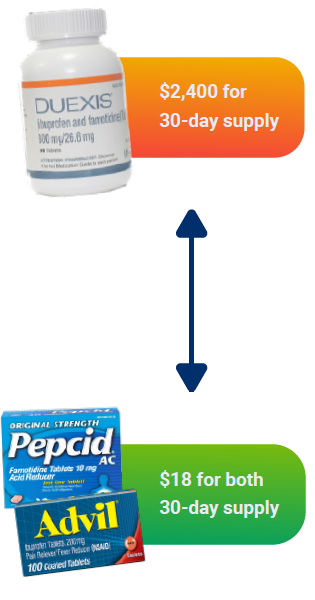
Low Clinical Value Formulary Exclusions – RxBenefits removed a combination medication known as Duexis® that was costing the plan $2,400 for a 30-day supply. In its place, members received over-the-counter-alternatives Advil® and Pepcid® that cost about $18 for a 30-day supply, achieving the same clinical outcome at a much lower cost.
High Dollar Claim Review – RxBenefits’ team of pharmacists reviewed the plan’s high-cost claims (those that exceed $1,000 per month) to determine their clinical necessity and identify any lower-cost alternatives. The plan’s three most expensive medications, Gattex®, Epclusa®, and Kalyeco®, accounted for a combined annual plan cost of more than $1.28M.
The Impact
The school board was able to reverse the trend of increasing prescription drug costs and deliver an improved pharmacy benefit program to its members by implementing a tailored combination of RxBenefits’ Protect strategies. Over the first half of the year, the school board decreased their average plan spend significantly — the LCV program alone provided an estimated savings or cost avoidance of $29,704, while the High Dollar Claim Review program produced an additional $120,880 in estimated savings on reviewable non-specialty high dollar claims, within the first six months of the year.
$150K savings
in plan cost avoidance in 6 months
$7.30 PMPM
reduction in average plan spend
from the LCV and High Dollar
Claim Review solutions

Originally published on: September 16, 2020
Updated on: December 19, 2023
