Straightforward Process, Results That Matter
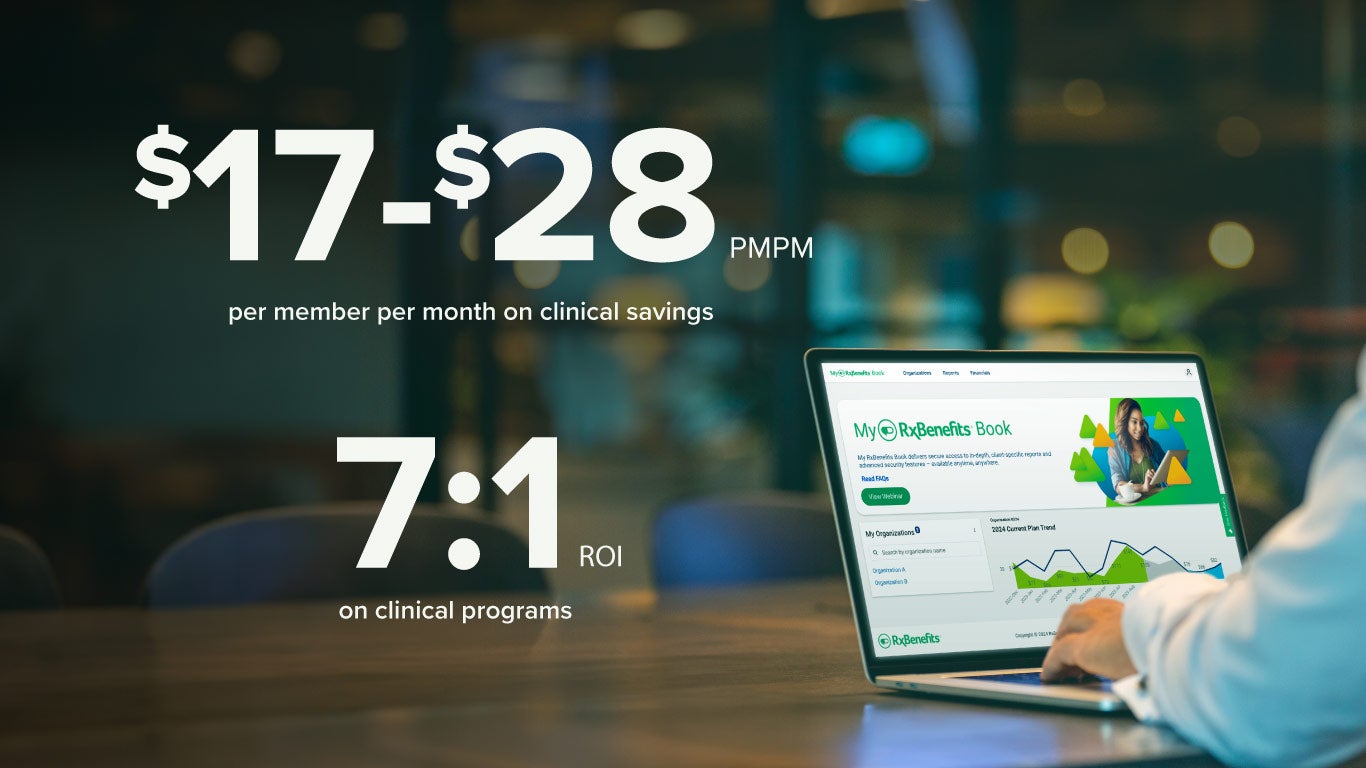
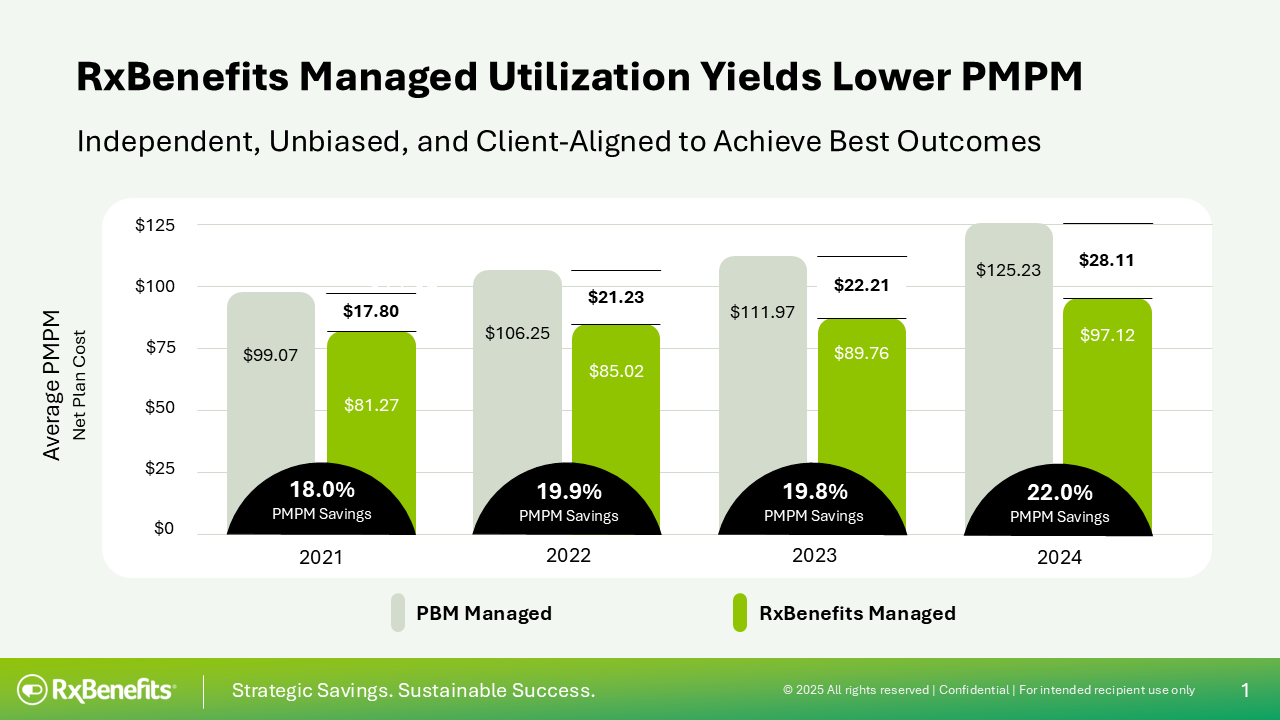
Our human-led, independent clinical utilization management uniquely positions us to deliver strategic savings. Our clients save an average of $17-$28 per-member-per-month (PMPM) clinical savings, which is 22% more than savings achieved when clinical is managed by traditional pharmacy benefits managers (PBMs)
These savings are possible because our pharmacy benefits optimizer (PBO) model is 100% client-aligned. We are not beholden to a single PBM or offering. We curated a best-in-class marketplace where traditional and transparent PBMs compete for our clients’ business. Our clients see an average 7:1 return on investment – $7 in clinical savings for every dollar they spend on our clinical management solutions. These are hard dollar savings.
Here’s how we do it:
- We begin by analyzing current plan economics, including utilization patterns and drug mix. Then we assess the client’s specific cost containment and member access goals. From there, we help clients choose the right solutions to meet their needs.
- Our PA reviews are conducted by independent clinicians, not automation, which reduces the risk of inappropriate, off-label, or unsafe prescriptions being filled. We focus on ensuring patients receive the right drug, at the right dose, at the lowest possible cost.
- Our pharmacists work collaboratively with providers, to optimize medication regimens for members with complex conditions, utilizing a peer-review process to improve clinical efficacy while reducing plan costs.
At RxBenefits, strategic savings and sustainable success are not just words, they are part of our core values and the guiding force that powers our mission of ensuring that every working American and their employer have access to quality prescription medications at an affordable cost.




